
There should be a specific person responsible for specific steps and a good team leader. The chances of a successful outcome depend on a very coordinated resuscitation process. Near pulseless electrical activity or a very low-output state may also be managed with circulatory assistance (e.g., intra-aortic balloon pump, extracorporeal membrane oxygenation, cardiopulmonary bypass, and ventricular assist device). In a patient with a refractory case and chest trauma, a thoracotomy may be performed. Pericardial drainage and emergent surgery may be lifesaving in appropriate patients with pulseless electrical activity.

Avoid routine administration of sodium bicarbonate as it worsens intracellular and intracerebral acidosis without affecting mortality.
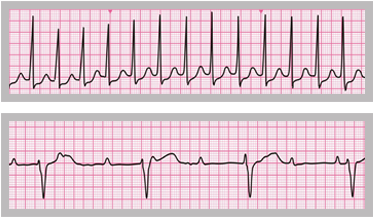
Sodium bicarbonate may be used only in patients with severe, systemic acidosis, hyperkalemia, or tricarboxylic acid overdose. Note that atropine may cause pupillary dilation therefore, this sign cannot be used to assess neurologic function. This is considered the optimal dose, beyond which no further benefit will occur. If the detected rhythm is bradycardia that is associated with hypotension, then atropine (1 mg IV every 3-5 min, up to three doses) should be administered. It can also be given via an endotracheal tube after mixing 2 mg in 10 ml of normal saline. Selected patients, like those with beta-blockers or calcium channel blockers overdose, may benefit from higher-dose epinephrine. Higher doses of epinephrine have not been shown to improve survival or neurologic outcomes in most patients. Each dose should be followed by 20 ml of flush and elevating the arm for 10 to 20 seconds for better perfusion. An arterial blood gas and serum electrolytes should be obtained during the resuscitation process.Įpinephrine should be administered in 1 mg doses intravenously (IV)/intraosseously (IO) every 3 to 5 minutes during pulseless electrical activity arrest. Once a diagnosis is made, begin immediate, specific management, i.e., decompression of pneumothorax, pericardial drain for tamponade, fluids infusion for hypovolemia, correction of body temperature for hypothermia, administration of thrombolytics for myocardial infarction or pulmonary embolism. The first step in managing pulseless electrical activity is to begin chest compressions according to the advanced cardiac life support (ACLS) protocol followed by administrating epinephrine every 3 to 5 minutes, while simultaneously looking for any reversible causes. Pulseless electrical activity can include a number of organized cardiac rhythms that may be supraventricular in origin, sinus versus non sinus, or ventricular in origin such as accelerated idioventricular or escape. An impalpable pulse should not always be taken as a pulseless electrical activity because it may be due to severe peripheral vascular abnormality. True pulseless electrical activity is a state in which cardiac contractions are lacking in the presence of coordinated electrical impulses.

There can be ventricular contractions and detectable pressures in the aorta, which are also known as pseudo-PEA. Pulseless electrical activity does not necessarily mean the lack of mechanical activity. The word “sufficient” is being used to describe a degree of ventricular mechanical activity that is adequate to generate a palpable pulse. In the case of cardiac arrest, the organized ventricular electrical activity does not usually follow sufficient ventricular response. It means that the electrical activity is pertinent, but not sufficient, condition for contraction. Pulseless electrical activity (PEA), also known as electromechanical dissociation, is a clinical condition characterized by unresponsiveness and impalpable pulse in the presence of sufficient electrical discharge. A lack of ventricular impulse often points to the absence of ventricular contraction, but the contrary is not always true.


 0 kommentar(er)
0 kommentar(er)
